The basis of the model
The StACC model is based on the five-steps established through the Health Foundation’s Co-creating Health Self-Management Programme (“SMP”) that ran from 2007 to 2012. This provides a structure that Health and Wellbeing Coaches can use to support self-management and increase activation, utilising the PCI-accredited core curriculum health coaching skills.
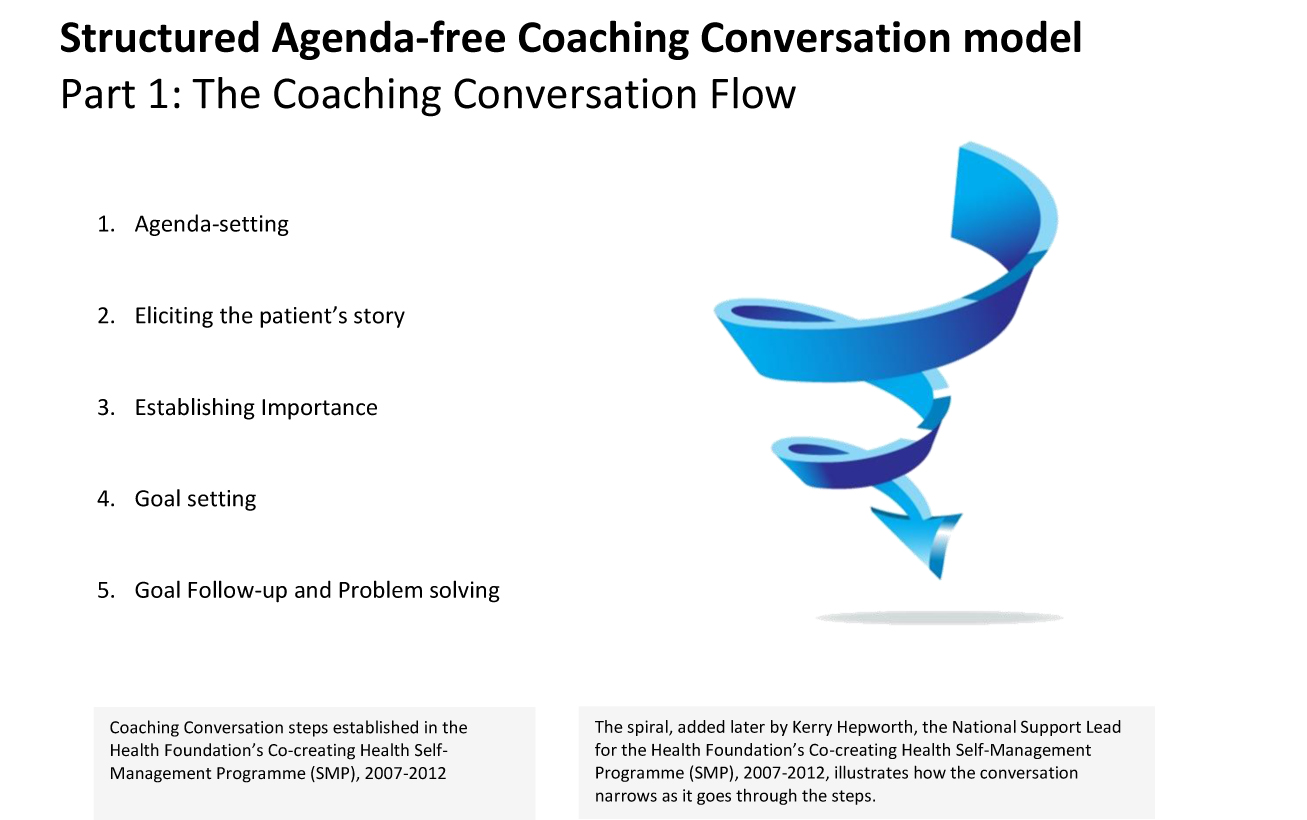
The structure is straightforward and easy to learn. The skill, in terms of using the steps for patient activation, is in being able to move flexibly, forwards and backwards, within the structure in order to meet the patient where they are at any time, using the skills appropriately at each stage.
How the model works to increase patient activation
‘Patient activation’ was defined by Hibbard and colleagues as ‘an individual’s knowledge, skill, and confidence for managing their health and health care’ (Hibbard et al, 2005), with the stages described as follows:
- believing the patient role is important,
- having the confidence and knowledge necessary to take action,
- actually taking action to maintain and improve one's health, and
- staying the course even under stress."
In the StACC model, these are abbreviated to:
- Importance (of own role),
- Confidence (to achieve goals)
- Problem-solving (when set-backs arise).
![The Structured Agenda-free Coaching Conversation model: What happens at each stage, with reference to patient activation levels [Hibbert et al, 2004]](https://kyoh.org/SiteUploads/91/Uploads/SACCmodel/Structured-Agenda-free-Coaching-Conversation-('StACC')-model---Diagram-2---Increasing-Activation--2-Sep-22.jpg)
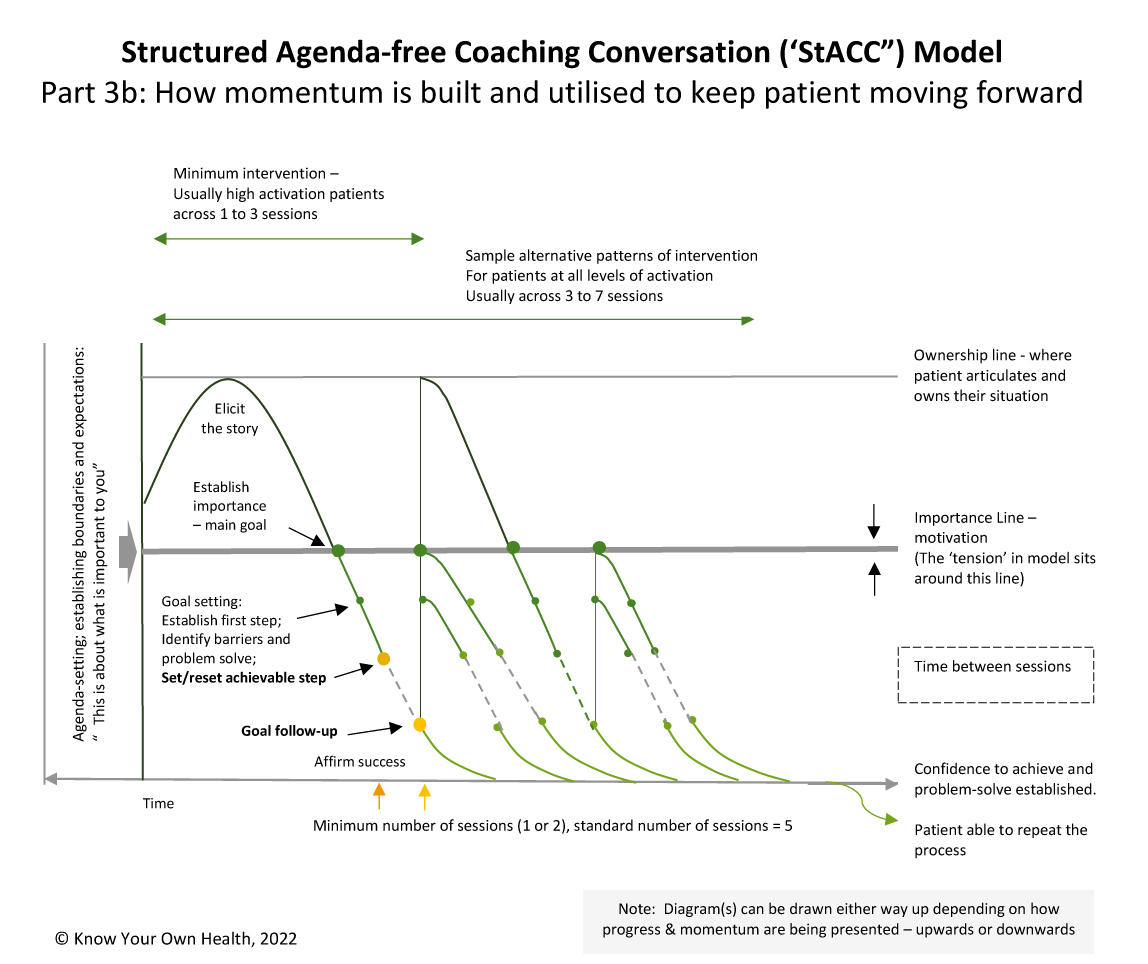
Moving through the steps of the Coaching Conversation enables movement through the activation levels.
The tension in the model sits around the ‘Importance line’ in the diagram.
This means the Coaching Conversation can be regarded as a process of two halves: One focused on the importance of the patient’s role and their sense of ownership, and one focused on action and their confidence to achieve their goals and problem-solve when setbacks arise.
Increasing activation is important as higher levels of activation are linked to better health and wellbeing outcomes for patients and reduced reliance on clinical services (Health Foundation, 2018).
How to use the model effectively
In the StACC model, patients are first ‘activated’ before moving to action. By being given ownership and control, patients are empowered to drive the agenda before being supported to set and achieve goals, building their knowledge, skills and confidence in the process. As a result, they are then able to internalise the process and apply it to other goals.
This differs from trying to build a patient’s knowledge, skills and confidence in the hope that they will become activated.
The model works for people at all levels of activation. What changes is the pace.
People at low levels of activation, or who are stuck or struggling, are likely to spend more time at the ‘top-end’ of the Coaching Conversation, i.e. Eliciting the Story, before moving to action than someone at high levels of activation who is more likely to move more quickly onto Goal-Setting and Problem-Solving.
This is because people at higher levels of activation are likely to already have a sense of ownership and level of confidence to achieve their goals. People at low levels of activation may therefore end up having a few more sessions than the standard 5 sessions plus a follow-up. See illustration, below:
-Model---Diagram-3a---Working-Flexibly---6th-September-22.jpg)
The skill is in using the PCI Core Curriculum skills and moving flexibly within the model. The patient’s journey may not be in a ‘straight line’ and the coach will need to move up and down the Coaching Conversation Flow, using the Structured Agenda-free Coaching Conversation model in order to meet the patient where they are at any one time and to move the patient forward from there. The diagram below illustrates how that works across time:
The model adjusts ‘SMART’ goals to ‘SMMART’ goals or, as expressed in the correct but less memorable order, ‘SMMTAR’ goals. These are SMART goals with Motivation added in alongside Specific, Measurable, Time-specific, Achievable and Realistic.